Alzheimer’s disease is a progressive mental decline affecting one’s memory and other cognitive functions. According to the Alzheimer’s Association (2016) there are over 5 million cases in the US each year and Alzheimer’s disease is the 6th leading Cause of death in the US.
Currently, there is no cure for Alzheimer’s disease, however exciting, cutting- edge research and observational studies find that along with early detection and specific diet and lifestyle interventions, it may be increasingly possible to prevent or slow the progression and even reverse the disease!

The Quality and Quantity of Sleep Matters
Alzheimer’s disease and age–related mental decline is characterized by the accumulation of amyloid plaques in the brain. Research tells us that a nutrient poor diet and poor sleep quality combined with insufficient physical activity and insufficient cognitive activity may all contribute to the early accumulation of such plaques in the brain related to Alzheimer’s. Dr. Tammy Scott, an expert from Tufts’ Neuroscience and Aging Laboratory states, “lifestyle factors such as diet, physical activity and quality of sleep are all possible risk factors for dementia.” In fact, independent of diet, poor sleep quality has been shown to be linked with a higher risk of Alzheimer’s; whereas getting 7-8 hours of good quality sleep allows for the brain to clear the amyloid plaques and “debris” that leads to Alzheimer’s.
A Healthy Diet that Improves Health, Sleep Quality and Lowers Risk of Alzheimer’s
Likewise, the Standard American Diet (SAD) along with a sedentary lifestyle can encourage the build-up of unwanted plaques affecting the brain. Experts suggest following a Mediterranean-style diet to help decrease one’s Alzheimer’s risk. Additionally, not only can a nutrient-dense Mediterranean –style diet help to deter Alzheimer’s risk, such dietary implementations can also influence the body’s cortisol levels and in turn promote improved sleep- also necessary as mentioned prior. A Mediterranean- style diet is characterized by eating primarily plant-based foods such as fruits, vegetables, legumes, nuts, and complex carbohydrates. It suggests eating a moderate amount of fish (at least twice a week) and having olive oil as the main source of fats, rather than butter, saturated fats, and fried food. The Mediterranean diet promotes using herbs and spices to season food rather than salt (Sofi et al., 2010).
More specific dietary suggestions to decrease Alzheimer’s risk include eating:
- At least 1-2 servings of dark leafy greens and/or vegetables a day
- Dark-colored berries: blueberries or blackberries which are loaded with antioxidants to decrease brain aging
- Nuts, which provide healthy fats and vitamin E. Specifically Brazil nuts which also contain selenium important for brain protection
- Beans, which provide a lot of fiber and help decrease inflammation in the body
- Lean protein like chicken or turkey which contain important amino acids required for proper neurotransmitter levels and proper cell signaling
- Fish like salmon, tuna, and trout containing Omega 3 fatty acids
- Other healthy fats like flaxseed, olive oil, and avocados/avocado oil in salads or dressings
Other key dietary components include limiting refined sugars and sweets and limiting consumption of grain-fed red meat to no more than a few times a month. Other key vitamins associated with protection against degenerative changes in the brain include Vit B12, B1, B3, Vit C, and Vit E.
Keep Your Body and Your Mind Active
Additional ways to boost cognitive health include: aiming for at least 30 minutes of physical activity a day and maintaining a healthy weight. Researchers have also linked diabetes to Alzheimer’s- type decline. It is also important to stay cognitively active via social engagement or by partaking in mentally stimulating activities like playing games, doing word searches, crossword puzzles, and reading or writing.
Promising research is developing in these areas. What we know for sure is early detection and prevention are key to minimizing one’s risk of Alzheimer’s disease. Supplemental Readings include: The Blue Zones Solution, by Dan Buettner and Keep Your Brain Alive by Lawrence C. Katz, PhD.
Keep Reading…
Easy Tips to Help Keep You Golfing All Summer
As nicer weather is hopefully approaching; it is that time [...]
What is Tennis Elbow?
What is Tennis Elbow? Tennis Elbow, or Lateral Epicondylitis, [...]
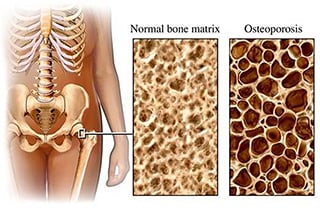
What is Osteoporosis?
What is Osteoporosis? Osteoporosis is a condition that causes [...]
The Truth about The Core and Balance
Most people equate having good strength to "six pack abs." The truth is that while it might look good, the six pack is not the same as having a strong core.
4 Quick Tips for Avoiding Hand Injuries
We live in a technology driven word, giving our hands, wrists and fingers more of a workout than we realize. A physical therapist can help prevent these types of overuse injuries.
Incontinence – Not the New Normal
With female incontinence being brought to the forefront by companies whose sole purpose is to make money on their products - it’s no surprise we’re being fed a lie about it being a “normal” transition of life.